Healthcare’s escalating costs and variable outcomes have long presented a formidable challenge. In response, a transformative approach has emerged: Value-Based Care (VBC). Unlike traditional models, VBC fundamentally redesigns how healthcare providers are reimbursed, linking payment directly to the value delivered – defined by quality, improved patient outcomes, and responsible cost management.
For organizations like payers, Managed Care Organizations (MCOs), and Accountable Care Organizations (ACOs), embracing this shift is crucial for long-term success. Join us as we dissect VBC and its alternatives, uncovering why value is becoming the industry’s new North Star.
The Incumbent: Fee-for-Service (FFS) – The Volume Game
For decades, the bedrock of healthcare payment has been the Fee-for-Service (FFS) model.1 Simple in its premise, it pays providers for each individual service rendered: every office visit, every lab test, every procedure.2
The Incentives (and Their Systemic Consequences):
From the perspective of a payer or MCO, FFS creates a treadmill of escalating costs. Providers are incentivized by volume; the more services they deliver, the more revenue they generate.3 This often leads to:
- Uncontrolled Cost Escalation: As payers, you bear the primary financial risk of unlimited service utilization, with little inherent leverage to manage total cost.4
- Reactive Care: The system rewards treating illness rather than preventing it.5 There’s minimal financial incentive for proactive care coordination, patient education, or wellness programs that might reduce the need for future, more expensive services.
- Fragmented Care: Providers often operate in silos.6 There’s no built-in financial reward for coordinating care across different settings or specialists, leading to duplicative tests and inefficient patient journeys.
- Difficulty in Quality Enforcement: While quality measures might exist, FFS doesn’t directly tie payment to outcomes, making it challenging for payers to ensure the value received for their expenditures.
For payers and MCOs, FFS historically meant a constant battle against rising expenditures with limited control over clinical outcomes. For providers looking to form ACOs, FFS provided no pathway for being rewarded for collective efficiency or quality improvements.
The Evolving Landscape: Pre-VBC Alternatives (and their limitations)
Before the comprehensive framework of VBC truly took hold, healthcare experimented with various payment models to address FFS’s shortcomings. While well-intentioned, these often came with their own limitations:
- Pure Capitation:
- How it worked: In its traditional form (think early HMOs), a provider or group received a fixed per-member-per-month (PMPM) payment to cover all care for an attributed patient, regardless of services used.
- Goals: Provided cost predictability for payers and a strong incentive for providers to manage utilization to stay profitable.
- Major Pitfall: Often lacked robust, enforceable quality oversight. The significant financial risk on the provider could, in some cases, create an incentive for under-serving patients if cost control overshadowed patient needs, eroding trust.
- Early Bundled Payments:
- How it worked: A single, global payment for a defined episode of care (e.g., a specific surgery, from pre-op to 90 days post-op).7
- Goals: Encouraged cost efficiency and coordination within that specific episode.
- Major Pitfall: While effective for episode costs, it often didn’t incentivize long-term patient management or broader population health. Its scope was limited to discrete events.
- Early Pay-for-Performance (P4P):
- How it worked: Small bonuses paid to providers for meeting specific, individual quality metrics (e.g., vaccination rates, basic chronic disease control).8
- Limitations: While a step towards quality, P4P often functioned as an add-on to FFS, not a true replacement. It didn’t significantly shift financial risk for overall cost or incentivize comprehensive care transformation.
These models were attempts to inject elements of value, but they often addressed only isolated aspects (cost control or specific quality points) without the holistic view that VBC now champions.
The Game Changer: Value-Based Care (VBC) – The Strategic Imperative
Value-Based Care is the culmination of these evolutionary steps, but with a critical difference: it brings together financial incentives, quality accountability, and comprehensive patient management into an integrated framework. It’s not just about paying less; it’s about paying smarter for better health.
Why VBC is Gaining Unstoppable Momentum:
For payers, MCOs, and ACOs, VBC isn’t merely an option; it’s a strategic imperative that directly addresses the shortcomings of older models:
- Sustainable Cost Management: VBC models shift financial risk (or create shared risk) to providers, powerfully incentivizing efficiency, waste reduction, and proactive prevention.9 Payers and MCOs gain greater predictability and control over expenditures.
- True Quality & Outcomes Focus: Reimbursement is directly tied to measurable improvements in patient health, safety, and experience. This elevates the discussion from procedure counts to readmission rates, chronic disease control, and patient satisfaction, aligning financial success with clinical excellence.
- Proactive & Preventive Health: The financial incentives in VBC heavily reward keeping patients healthy and out of costly acute care settings.10 This drives investment in wellness programs, chronic disease management, and timely screenings.
- Integrated & Coordinated Care: VBC fundamentally encourages collaboration. ACOs are designed to break down silos between primary care, specialists, hospitals, and post-acute care, leading to seamless transitions and reduced duplicative services.11 MCOs can build networks of high-performing, coordinated providers.
- Population Health Management at Scale: VBC enables payers and ACOs to take responsibility for the health of entire defined populations, identifying at-risk individuals, managing care gaps, and deploying targeted interventions.
In essence, VBC transforms the relationship:
- For Payers & MCOs: From passively absorbing costs to actively investing in the health of their members and driving value from their provider networks.
- For ACOs: From simply delivering services to becoming accountable health managers, empowered to innovate and share in the savings their holistic care generates.
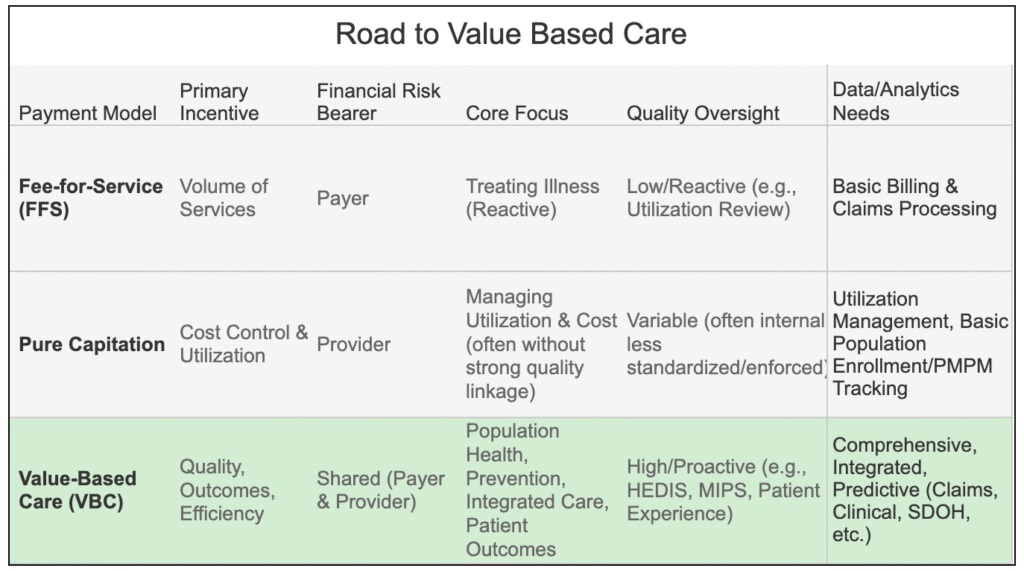
VBC vs. Alternatives: A Visual Comparison
Here’s a snapshot of how Value-Based Care strategically contrasts with its alternatives:
The Indispensable Role of Analytics & Visualization in This Transition
The shift from FFS to VBC is not merely a change in payment; it’s a fundamental transformation of operations, incentives, and accountability.12 And at the heart of this transformation lies data.
For payers, MCOs, and ACOs, navigating and succeeding in VBC is impossible without:
- Robust Data Aggregation: Pulling together claims, clinical, pharmacy, and even social determinants of health data.
- Sophisticated Analytics: Identifying risk, stratifying populations, predicting outcomes, and pinpointing cost drivers.13
- Crucially, Strategic Data Visualization: Translating complex analytical findings into clear, compelling, and actionable insights that empower executive decisions, guide clinical interventions, and demonstrate the tangible benefits of VBC to all stakeholders.
It’s about moving beyond simply reporting numbers to truly understanding the value created.
The Future is Value.
As the healthcare landscape continues its rapid evolution towards value, the ability to analyze, understand, and, most importantly, visualize performance within these new models will determine success. In our upcoming posts, we’ll dive deeper into specific VBC payment models and explore practical visualization techniques that empower your organization to thrive.